Trigeminal Neuralgia
Trigeminal Neuralgia
(Facial Pain
What you need to know about
Trigeminal Neuralgia
Trigeminal neuralgia is a severe facial discomfort that occurs suddenly. It’s typically described as a sudden shooting pain in the jaw, teeth, or gums, or as an electric shock.
It normally occurs in brief, unpredictable attacks that last anywhere between a few seconds and two minutes. The attacks end as quickly as they began.
Trigeminal neuralgia usually affects only one side of the face, with pain originating in the lower region of the face. Pain can strike both sides of the face on rare occasions, but not always at the same moment.
People who have the illness may have pain attacks on a daily, weekly, or monthly basis. Attacks might occur hundreds of times per day in severe situations.
Pain can improve or even go away for months or years at a time (remission), though these times tend to get shorter over time.
Some people may experience a constant aching, throbbing, or burning sensation, which may or may not be accompanied by sharp assaults.
It’s difficult to live with trigeminal neuralgia. It can have a major impact on a person’s quality of life, leading to issues like weight loss, solitude, and despair.
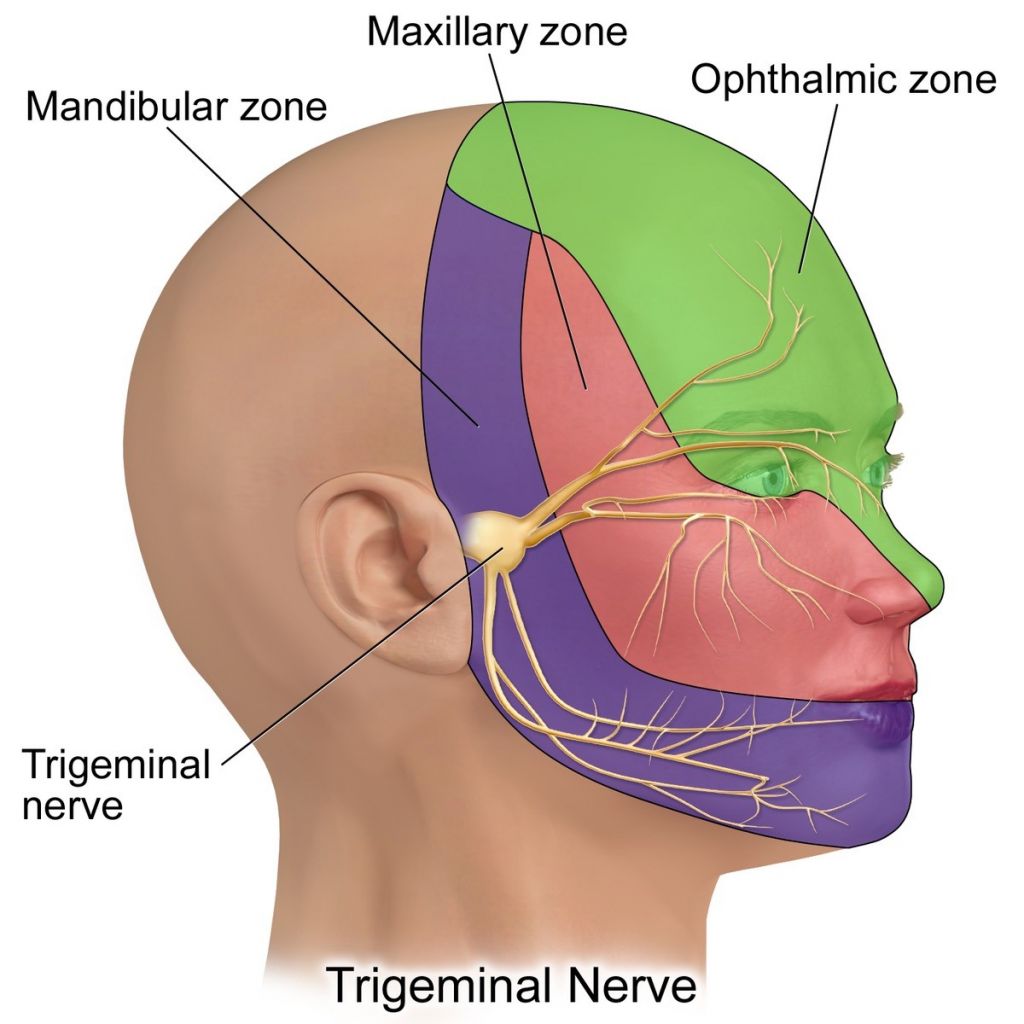
Mapping the Nerves in Your Face
It helps to understand how the afflicted nerves are laid out when learning about trigeminal neuralgia.
There are 12 pairs of what are known as cranial nerves in your head. These nerves include the trigeminal nerves, which allow you to feel sensations on your face. Each side of your head has one nerve.
Each trigeminal nerve has three branches that control different aspects of your facial sensation. They’re as follows:
- The ophthalmic branch. It is in charge of the eye, top eyelid, and forehead.
- The maxillary branch. The lower eyelid, cheek, nostril, upper lip, and upper gum are all affected.
- The mandibular branch. It controls your jaw, lower lip, lower gum, and some chewing muscles.
Symptoms of Trigeminal neuralgia
Trigeminal neuralgia is characterised by sudden occurrences of intense, sharp, shooting face pain that last anywhere from a few seconds to two minutes.
Excruciating pain, similar to an electric shock, is frequently recounted. You may be unable to accomplish anything while the attacks are occurring because they are so terrible.
One side of the face is frequently affected by trigeminal neuralgia. It can affect both parties in some circumstances, although not always at the same time.
Teeth, lower jaw, upper jaw, or cheek pain are all possibilities. Pain in the forehead or eye can occur less frequently.
Although most attacks start suddenly, you may detect when one is about to happen.
A small discomfort or burning sensation may occur after the most intense pain has faded. Between attacks, you may experience a persistent throbbing, aching, or burning sensation.
You may have recurring pain bouts that last for days, weeks, or months. Pain can sometimes go away completely and not return for months or even years. This is referred to as remission.
Trigeminal neuralgia bouts can occur hundreds of times per day in extreme cases, with no periods of remission.
Triggers
Trigeminal neuralgia attacks can be provoked by a variety of motions or movements, including:
- Talking
- Smiling
- Chewing
- Brushing your teeth
- Washing your face
- A light touch
- Shaving or putting on make-up
- Swallowing
- Kissing
- A cool breeze or air conditioning
- Head movements
- Vibrations, such as walking or travelling in a car
Pain, on the other hand, might occur without any apparent cause.
Diagnosis
Trigeminal neuralgia pain is frequently felt in the jaw, teeth, or gums, so many patients with the illness see a dentist before seeing a doctor.
To help them analyse your facial pain, the dentist will ask you about your symptoms and take a dental X-ray. They’ll check for things like a dental infection or a damaged tooth, which are common causes of facial pain.
Trigeminal neuralgia is frequently diagnosed by a dentist, but if your dentist has found no obvious cause for your discomfort, you should see a doctor.
Excluding other possibilities
Trigeminal neuralgia pain is frequently felt in the jaw, teeth, or gums, so many patients with the illness see a dentist before seeing a doctor.
To help them analyse your facial pain, the dentist will ask you about your symptoms and take a dental X-ray. They’ll check for things like a dental infection or a damaged tooth, which are common causes of facial pain.
Eliminating other illnesses that cause facial discomfort is an important aspect of the trigeminal neuralgia diagnosis procedure.
The GP may be able to rule out other disorders by asking about your symptoms and performing an examination, such as:
- Migraine
- Joint pain in the lower jaw
- Giant cell arteritis (temporal arteritis) – where the medium and large arteries in the head and neck become inflamed and cause pain in the jaw and temples
- A possible nerve injury
When trying to figure out what’s causing your pain, your doctor will inquire about your medical, personal, and family background.
If you’re under 40 years old, you’re less prone to have trigeminal neuralgia. If you have a family history of multiple sclerosis (MS) or have another form of the disease, MS may be a more likely cause.
Trigeminal neuralgia, on the other hand, is unlikely to be the first symptom of MS.
MRI scans
If your doctor is unsure about your diagnosis or you have odd symptoms, you may be referred for a head MRI scan.
An MRI scan creates detailed images of the inside of your body using strong magnetic fields and radio waves.
It can help you figure out what’s causing your facial pain, such as sinusitis (inflammation of the sinus lining), tumours on one of your facial nerves, or nerve damage caused by MS.
An MRI scan can also reveal whether a blood artery in your head is crushing one of your trigeminal nerves, which is the most common cause of trigeminal neuralgia.
Causes
Compression of the trigeminal nerve is the most common cause of trigeminal neuralgia. This is the nerve that runs through your skull and transmits pain and touches sensations from your face, teeth, and mouth to your brain.
An adjacent blood artery compressing a portion of the trigeminal nerve inside the skull is the most common cause of the compression.
Trigeminal neuralgia can also be caused by another medical illness, such as multiple sclerosis (MS) or a tumour, which damages the trigeminal nerve.
Pain can be provoked by wind – even a modest breeze or air conditioning – or movement of the face or head. Pain can occur without any apparent cause.
Although the specific aetiology of trigeminal neuralgia is unknown, it is frequently assumed to be caused by compression of the trigeminal nerve or another medical problem affecting this nerve.
The trigeminal nerve, often known as the fifth cranial nerve, is responsible for facial feeling. On each side, you have one.
Primary trigeminal neuralgia
Evidence suggests that pressure on the trigeminal nerve around where it enters the brain stem, the lowest region of the brain that joins with the spinal cord, causes trigeminal neuralgia in up to 95% of cases.
Primary trigeminal neuralgia is the most common kind of trigeminal neuralgia.
An artery or vein squashing (compressing) the trigeminal nerve is the most common cause of pressure. These are ordinary blood arteries that come into contact with a nerve at a highly sensitive location.
Because not everyone with a compressed trigeminal nerve will experience pain, it’s unclear why this pressure can trigger painful attacks in some people but not others.
It’s possible that pressure on the nerve wears away the protecting outer layer (myelin sheath) in certain persons, allowing pain signals to pass along the nerve. This does not, however, explain why some people experience periods without symptoms (remission) or why pain relief is immediately following a successful operation to shift blood vessels away from the nerve.
Secondary trigeminal neuralgia
When trigeminal neuralgia is caused by another medical illness or problem, it is referred to as secondary trigeminal neuralgia, these include:
- A tumour
- a cyst, a fluid-filled sac in the body.
- A unique tangle of arteries and veins is known as an arteriovenous malformation.
- Multiple sclerosis (MS) is a chronic disease that affects the neurological system.
- Face trauma
- Surgery-related damage, including dental surgery
Complications
Living with trigeminal neuralgia is challenging, and your quality of life can suffer as a result.
You may feel compelled to avoid tasks like cleaning, shaving, or eating in order to avoid triggering the pain, and your fear of suffering may cause you to avoid social situations.
However, it’s critical to maintain a normal lifestyle and to be conscious that being undernourished or dehydrated can exacerbate the pain.
Living with chronic pain can cause emotional strain, which can lead to psychological issues like depression. Some people may even ponder suicide during instances of acute discomfort. You may live in terror of the pain returning even while you are pain-free.
When to call a doctor
If you have regular or persistent facial discomfort, see a doctor, especially if over-the-counter painkillers like paracetamol and ibuprofen don’t work and a dentist has ruled out any dental causes.
The diagnosis of trigeminal neuralgia is complicated. The doctor will try to figure out what’s wrong by asking you about your symptoms and ruling out any other possible causes for the pain.
Because there is no specific test for trigeminal neuralgia, it is usually diagnosed solely on your symptoms and pain description.
If you’ve had attacks of facial pain, your doctor will ask you questions about them, such as:
- How frequently do pain attacks occur?
- How long do the pain assaults persist, and what parts of your face are affected?
- Other probable reasons for your discomfort will be considered, and your GP may examine your head and jaw to determine which regions are uncomfortable.
Treatment
There are several treatments that can help with the pain produced by trigeminal neuralgia.
Identifying and avoiding triggers can also be beneficial.
The majority of patients with trigeminal neuralgia will be prescribed medication to help them manage their pain, although surgery may be considered in the long run if medication is ineffective or produces too many negative effects.
Try to avoid triggers
Trigeminal neuralgia attacks can be triggered or exacerbated by particular triggers, thus avoiding them as much as possible may be beneficial.
If your pain is triggered by wind, for example, wearing a scarf across your face in windy weather may assist. A transparent dome-shaped umbrella can help keep the rain off your face.
Avoid sitting near open windows or the source of air conditioning if your pain is provoked by a draught in a room.
If hot, spicy, or cold foods or drinks seem to aggravate your pain, avoid them. Drinking warm or cold beverages with a straw might help avoid the liquid from coming into touch with uncomfortable parts of your mouth.
If you’re having trouble chewing, try soft foods or liquidising your meals.
Certain foods, such as caffeine, citrus fruits, and bananas, appear to cause attacks in some people, so you may wish to avoid them.
Medication
Because paracetamol is ineffective in treating trigeminal neuralgia, an anticonvulsant, a type of medicine used to treat epilepsy, will be provided to assist you to manage your pain.
Anticonvulsants were not meant to treat pain, but they can help relieve nerve pain by decreasing electrical impulses in the nerves and diminishing their ability to transmit pain signals.
They must be taken on a daily basis, not just when pain attacks occur, but they can be stopped if the pain episodes stop and you are in remission.
It’s vital to gradually raise your dosage unless your doctor or an expert advises you otherwise. You can gradually reduce the dosage over the course of a few weeks if the pain goes away. Taking too much medicine too soon or discontinuing it too soon can lead to serious complications.
Initially, the GP will likely prescribe carbamazepine as an anticonvulsant, but if this proves ineffective or unsuitable, a variety of other anticonvulsants are available.
Carbamazepine
In the United Kingdom, the anticonvulsant carbamazepine is the sole drug approved to treat trigeminal neuralgia. It can be quite effective at first, but it may lose effectiveness over time.
Carbamazepine is normally started at a low dose once or twice a day, then gradually raised to up to four times a day until it gives sufficient pain relief.
Carbamazepine has a lot of adverse effects, which can make it difficult to take for some people.
These include:
- Tiredness and sleepiness
- Dizziness (lightheadedness)
- Difficulty concentrating and memory problems
- Confusion
- Feeling unsteady on your feet
- Feeling and being sick
- Double vision
- A reduced number of infection-fighting white blood cells (leukopenia)
- Allergic skin reactions, such as hives (urticaria)
If you have any persistent or bothersome side effects while taking carbamazepine, especially allergic skin responses, you should consult your doctor immediately.
Carbamazepine has also been related to a number of less common but potentially fatal adverse effects, such as suicidal ideation.
Any suicidal thoughts should be immediately reported to a doctor. Call NHS 111 if this isn’t possible.
Other medication
Carbamazepine may become ineffective over time. You should be referred to a specialist in this situation, or if you develop major side effects while taking it, so that alternate drugs or procedures can be considered.
You may be sent to a variety of specialists for additional therapy, including headache specialists, neurosurgeons, and pain medicine specialists.
Other drugs, in addition to carbamazepine, have been used to treat trigeminal neuralgia, including:
- Oxcarbazepine
- Lamotrigine
- Gabapentin
- Pregabalin
- Baclofen
None of these drugs have been specially approved for the treatment of trigeminal neuralgia, which means they haven’t been through rigorous clinical testing to see if they’re effective and safe.
Many doctors, however, will prescribe an unlicensed prescription if they believe it will be beneficial and the advantages of treatment will outweigh the hazards.
If your doctor recommends an unlicensed prescription to treat your trigeminal neuralgia, they should tell you that it’s unlicensed and go over the risks and benefits with you.
Most of these medications have side effects that might be difficult to deal with at first.
Although hardly everyone has adverse effects, if you do, keep trying because they usually fade with time or at least until the next dosage increase.
If the side effects are bothering you, talk to your doctor.
Surgery
If medication does not effectively control your symptoms or causes persistently bothersome side effects, you may be sent to a specialist to explore your surgical and non-surgical options.
There have been a variety of techniques done to treat trigeminal neuralgia, so talk to your doctor about the benefits and dangers of each one before deciding.
None of these methods can guarantee that they will work for you. If the procedure is successful, you will not require pain medication again until the discomfort returns.
If one procedure fails, you can attempt another or continue taking medications for the time being or permanently.
The following are some of the methods that can be used to treat trigeminal neuralgia.
Percutaneous procedures
By introducing a needle or thin tube through the cheek and into the trigeminal nerve inside the skull, a number of operations can provide some relief from the discomfort of trigeminal neuralgia, at least temporarily.
Percutaneous procedures are what they’re called. While you’re highly sedated with drugs or unconscious under a general anaesthetic, X-rays of your head and neck are taken to help guide the needle or tube into the precise position.
The following are percutaneous techniques for treating trigeminal neuralgia:
- Glycerol injections. Glycerol is injected around the Gasserian ganglion, which is where the three main branches of the trigeminal nerve meet.
- Radiofrequency lesioning. Where heat is applied directly to the Gasserian ganglion using a needle
- Balloon compression. Where a little balloon is delivered through a narrow tube put through the cheek The balloon is then inflated around the Gasserian ganglion to compress it before being removed.
These procedures act by injuring or disrupting the trigeminal nerve, causing pain signals to be disrupted. You can usually return home the next day.
Overall, these procedures are helpful at relieving trigeminal neuralgia pain, albeit each has its own set of risks. These can differ based on the technique and the person.
The pain reduction normally only lasts a few years or months in some circumstances. These operations aren’t always successful.
The most common adverse effect of these treatments is numbness on one side of the face, which can range from total numbness to pins and needles.
The sensation, which can be permanent, is often compared to the sensation you get after dental injection. Anaesthesia Dolorosa, a mix of numbness and chronic agony that is essentially untreatable, is also possible, but it is extremely unusual.
Other short- and long-term adverse effects and risks of these treatments include bleeding, facial bruising, vision issues, and hearing loss on the affected side. It can induce a stroke in rare cases.
Stereotactic radiosurgery
Stereotactic radiosurgery is a relatively recent technique in which a concentrated beam of radiation is used to intentionally damage the trigeminal nerve where it enters the brainstem.
There is no need for general anaesthesia with stereotactic radiosurgery, and no cuts (incisions) are made to your cheek.
A metal frame is affixed to your head, and four pins are placed into your scalp with a local anaesthetic to numb the locations where they are inserted.
While the radiation is provided, your head, including the frame, is held in a big machine for 1 to 2 hours. After a little rest, the frame and pins are removed, and you are free to return home.
After stereotactic radiosurgery, it can take a few weeks – or even months – to detect any changes, but it can provide pain relief for some patients for months or even years.
The most common side effects of stereotactic radiosurgery include facial numbness and pins and needles in the face. These adverse effects can last a long time and be highly bothersome in some circumstances.
Microvascular decompression
Microvascular decompression (MVD) is a procedure that can help reduce trigeminal neuralgia discomfort without causing permanent damage to the nerve.
Blood veins that are contacting or wrapped around the trigeminal nerve put pressure on it, therefore the operation relaxes it.
MVD is a major surgery that entails opening the skull and is performed by a neurosurgeon under general anaesthesia.
A little portion of skull bone is removed through an incision in your scalp, behind your ear. They then use a prosthetic cushion or a sling made from adjacent tissue to remove the blood vessel(s) from the trigeminal nerve.
Many people report that this surgery relieves or totally eliminates their trigeminal neuralgia pain.
It provides the longest-lasting relief, with some research suggesting that 3 out of 10 cases of pain return after 10 to 20 years post-surgery.
MVD is currently the most effective treatment for trigeminal neuralgia. However, because it’s an intrusive surgery, there’s a chance of major side effects like facial paralysis, hearing loss, stroke, and even death in about one out of every 200 instances.
Outlook
It’s difficult to live with a long-term, painful ailment like trigeminal neuralgia.
Contacting a local or national support organisation, such as the Trigeminal Neuralgia Association UK, for further information and guidance about living with the condition, as well as connecting with other individuals who have the condition to chat to about their experiences, may be beneficial.
There are several research efforts underway in the UK and overseas to discover the aetiology of trigeminal neuralgia and develop new therapies and drugs, so there is reason to be optimistic.


