Testicular Cancer
Testicular Cancer
SPREADING | RISK FACTORS | TREATMENT |
COMPLICATIONS | SUMMARY
EVERYTHING YOU NEED TO KNOW
ABOUT TESTICULAR CANCER
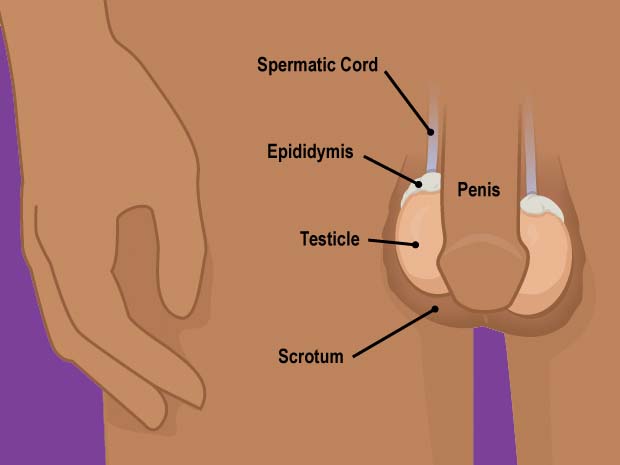
Testicular cancer is a type of cancer that starts in one or both of the testicles, or testes.
The testes are the male reproductive glands that are found inside the scrotum, which is the skin pouch beneath the penis. Sperm and the hormone testosterone are produced in the testes.
Anyone with testicles, including transgender and nonbinary people, can develop testicular cancer. Testicular cancer is a relatively uncommon kind of cancer in men, accounting for only 1% of all cancers. Each year, approximately 2,300 males in the United Kingdom are diagnosed with testicular cancer.
Germ cell alterations are the most common cause of testicular cancer. These are the sperm-producing cells in your testicles. About 95 percent of testicular malignancies are germ cell tumours.
Germ cell cancers are divided into two types:
Seminomas. These are slow-growing testicular tumours. They’re normally limited to your testes, but they can also affect your lymph nodes.
Nonseminomas. The most prevalent type of testicular cancer is this. This type grows more quickly and has the potential to spread to other places of your body.
Testicular cancer can also develop in hormone-producing organs. Gonadal or sex-cord stromal tumours are the names given to these tumours.
Testicular cancer is the most frequent malignancy in men between the ages of 15 and 49, but it can strike at any age. Even if it has spread to other parts of the body, it is one of the most curable malignancies.
Symptoms of testicular cancer
When testicular cancer is diagnosed, some patients experience no symptoms. When symptoms do arise, they may include the following:
- A mass in the testes
- Testicular discomfort or pain
- Testicular swelling
- Back or lower abdominal ache
- Lower belly ache or heaviness
- Breast tissue enlargement
- In prepubescent people with testicles, vocal alterations and face and body hair growth are common
Symptoms in the late stages
The following are some of the signs and symptoms of advanced testicular cancer:
- Cancer has progressed to the lymph nodes in the rear of the abdomen, causing low back pain.
- Breathing problems
- Chest discomfort
- Cough
- Stomach ache
- Headaches
- Confusion
If you have any of these symptoms, make an appointment with your GP.
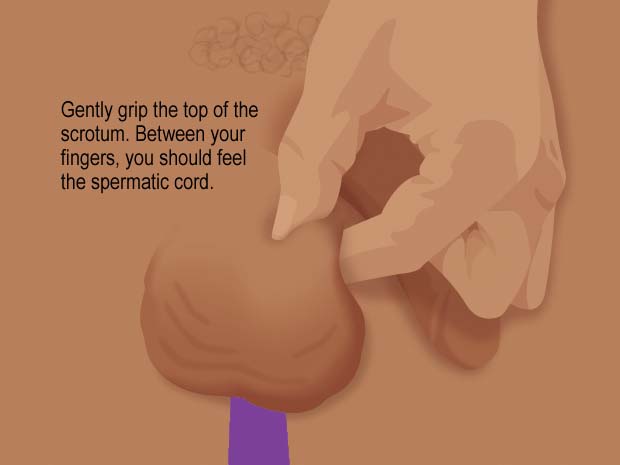
How to do a self-examination for testicular cancer
Self-examination of the testicles is a simple approach to check for malignancy. It is advised that testicles be self-examined once a month, so you become familiar with the size and shape of your testicles. Because your scrotum skin will be relaxed, the optimum time to examine your testicles is during or after a bath or shower.
Pick the best time to take your exam. It’s ideal to do it just after or during a hot shower or bath.
The scrotum (the skin that covers the testicles) is at its most loose during this time, making it simpler to feel for bumps in the testicles.
Lumps can be the size of a grain of rice or a pea.
Examine each testicle separately.
Begin by lightly grasping the top of the scrotum with your thumb on top and your fingers underneath. Pinch gently to keep the testicle in place and prevent it from moving during the exam.
You should be able to feel the spermatic cord between your fingers. The testicle is connected to the rest of your body by this.
Glide your thumb and fingers over both sides of the testicle, from top to bottom, with your free hand. Look for lumps and bumps.
Then run your fingertips over the testicle’s front and rear.
The epididymis, a tube that carries sperm, should be felt on the back at the top. This is a common bump that may be sensitive when touched.
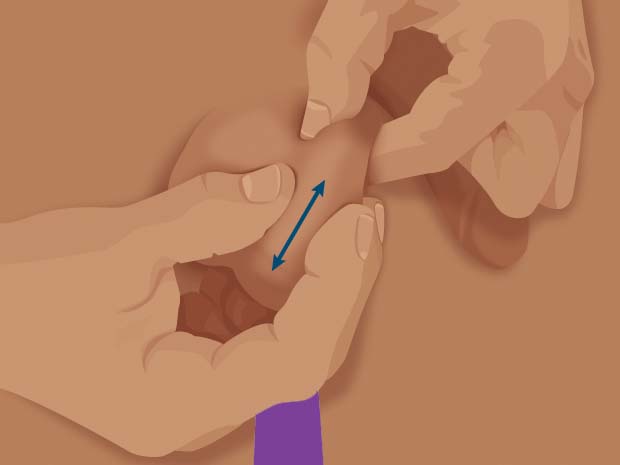
If you observe any swelling, lumps, or changes in the size or colour of a testicle, call your doctor straight away. If you have any pain or achy places in your groyne, tell your doctor.
It’s conceivable that lumps or swelling aren’t cancer, but they should be evaluated by a doctor as soon as possible.
If diagnosed and treated early, testicular cancer is almost usually curable.

How can you know if you have testicular cancer?
The following tests may be used by your doctor to diagnose testicular cancer:
- A physical examination that can identify any abnormalities in the testicles, such as tumours or swelling
- An ultrasound to evaluate the testicles’ internal structure
- Tumour marker tests are blood tests that can reveal high levels of chemicals linked to testicular cancer, such as alpha-fetoprotein or beta-human chorionic gonadotropin
If an ultrasound and blood tumour marker test reveals that you have testicular cancer, your doctor will most likely propose surgery. The treatment, known as a radical inguinal orchiectomy, tries to remove the tumour as quickly as possible so that a biopsy can be performed.
Cancer is diagnosed through biopsies. A biopsy of a testicular tumour can result in cancer spreading. As a result, your doctor will almost certainly remove the entire testicle from the scrotum in order to obtain a sample from the tumour.
Following the diagnosis, procedures such as pelvic and abdominal CT scans will be performed to detect if cancer has spread to other parts of the body. This is referred to as staging.
The following are the stages of testicular cancer:
- Stage 1 is limited to the testicle.
- Stage 2 has spread to lymph nodes in the abdomen.
- Stage 3 has spread to other parts of the body. This type of cancer can spread to the lungs, liver, brain, and bone.
The cancer is also classified according to how well it is predicted to respond to treatment. The prognosis can be positive, neutral, or negative.
Physical examination
A GP will normally need to examine your testicles in addition to interviewing you about your symptoms and reviewing your medical history.
They may shine a small light or torch against your scrotum to see if it reflects light.
Because testicular tumours are usually solid, light cannot flow through them.
Light will be able to flow through a collection of fluid in the scrotum.
Tests for testicular cancer
A GP will normally need to examine your testicles in addition to interviewing you about your symptoms and reviewing your medical history.
They may shine a small light or torch against your scrotum to see if it reflects light.
Because testicular tumours are usually solid, light cannot flow through them.
Light will be able to flow through a collection of fluid in the scrotum.
Ultrasound of the scrotum
A scrotal ultrasound scan is a painless treatment that produces an image of the inside of your testicle using high-frequency sound waves.
It’s one of the most common ways to determine if a mass is cancerous (malignant) or not (benign).
Your specialist will be able to assess the location and size of the abnormalities in your testicle through a scrotal ultrasound.
It will also reveal whether the lump is in the testicle or separate within the scrotum, as well as whether it is solid or fluid-filled.
The majority of the time, a fluid-filled lump or accumulation around the testis is innocuous. A firmer lump could indicate that the growth is malignant.
Blood tests
A series of blood tests to detect particular hormones in your blood, known as markers, may be required to help confirm a diagnosis.
These markers are frequently produced by testicular cancer, therefore finding them in your blood may indicate that you have the disease.
The following markers in your blood will be tested:
- Fetoprotein alpha (AFP)
- Human chorionic gonadotrophin (HCG)
A third blood test is frequently performed since it can reveal how aggressive malignancy is.
Lactate dehydrogenase (LDH) is a testicular cancer marker, but it isn’t specific.
Testicular cancer patients do not all generate indicators. Even if your blood test results are normal, there’s still a chance you have testicular cancer.
Histology
Examining a portion of the lump under a microscope is the only technique to clearly establish testicular cancer. Histology is the term for these tests and reports.
Unlike many malignancies, where a little bit of cancer can be removed (a biopsy), a testicular mass is usually only examined by totally removing the affected testicle.
This is due to the fact that a combination of ultrasound and blood marker testing is generally enough to make a definitive diagnosis.
A biopsy may also cause damage to the testicle, spreading malignancy to the scrotum, which is typically unaffected.
Only if your doctor is fairly convinced the lump is cancerous will he or she consider removing your testicle.
The loss of a testicle has no bearing on your sexual life or ability to conceive children.
An orchidectomy is the surgical removal of a testicle. It’s the most common therapy for testicular cancer, so if you have it, you’ll almost certainly need an orchidectomy.
Other tests
In virtually all cases, additional testing will be required to determine whether testicular cancer has spread.
When testicular cancer spreads, the lymph nodes in the rear of the abdomen or the lungs are most usually affected.
A chest X-ray may be required to check for evidence of a tumour.
A scan of your entire body is also required. A CT scan is frequently used to look for evidence of cancer spreading.
Another form of scan known as an MRI scan may be used in rare instances.
Stages of testicular cancer
It’s usually feasible to tell the stage of your cancer after all tests have been done.
Testicular cancer can be staged in two different ways.
The first uses a three-stage mechanism. The phases are determined by the extent to which the disease has progressed as well as the presence of substances linked to cancer (markers) in your blood.
Stage 1 testicular cancer is when the cancer is contained within your testicle.
Stage 2 testicular cancer is when cancer has spread into nearby lymph nodes (small glands that fight infection) in your pelvis or tummy.
Stage 3 cancer is split into 3 sub-stages.
When testicular cancer has migrated to distant lymph nodes, such as those near your collarbone or your lungs, it is called stage 3A. Your marker levels are either normal or slightly elevated.
There are two types of testicular cancer at stage 3B:
- You have greater marker levels because the malignancy has migrated to surrounding lymph nodes, or
- You have greater marker levels because cancer has migrated to distant lymph nodes or your lungs.
- Cancer spreads similarly to stage 3B testicular cancer, but you have very high marker levels or cancer has spread to another one of your body organs, such as the liver or the brain.
The TNM staging system is the second system, which is not extensively used in the UK:
- T denotes the tumour’s size.
- N indicates whether cancer has spread to nearby lymph nodes
- M indicates whether cancer has spread to other parts of the body (metastasis)
How fast does it spread?
Testicular cancer can spread to other areas of the body, such as the lungs, lymph nodes, liver, and brain, which is known as metastasis. The speed with which cancer spreads is determined by the sort of cancerous tumour you have and the “grade” in which your cancer cells are.
The following are the two most prevalent kinds of testicular cancer:
- Seminoma tumours develop at a slower rate than non-seminoma tumours. Seminoma tumours are more commonly discovered in the testicles, and they are less likely to migrate to other regions of the body.
- Non-seminoma tumours are more aggressive and spread more quickly than seminoma cancers. Nonseminoma cancers have a tendency to spread lymphatically, meaning they can reach the lymph nodes.
When a doctor takes a biopsy, they will examine the cancer cells and “grade” them on a scale of 1 to 3 based on how similar they appear to normal cells. Grade 3 cells have a distinct appearance from normal cells and develop and spread more quickly than grade 1 or 2 cells.
You might ask your GP to describe your cancer’s grade to you so you can figure out how soon cancer will spread.
Stages of testicular cancer
Testicular cancer can be caused by a number of factors, including:
- Having a history of the disease in one’s family
- Testicular development that is aberrant
- Being a white person
- Cryptorchidism is the condition of having an undescended testicle.
Treating testicular cancer
The three basic treatments for testicular cancer are chemotherapy, radiation, and surgery.
Your treatment plan will be determined by the following factors:
- Whether you have a seminoma or a non-seminoma kind of testicular cancer
- Your testicular cancer stage
Surgical removal of the afflicted testicle is the first therapeutic choice for all cases of testicular cancer, regardless of the stage (an orchidectomy).
After the testicle has been removed for stage 1 seminomas, a single dose of chemotherapy may be given to help prevent the cancer from returning.
A brief course of radiation may be suggested in some cases.
However, while the chances of recurrence are modest in many situations, your doctors may advise that you be closely monitored for the next few years.
Only a small percentage of patients who experience a recurrence require additional therapy.
Close follow-up (surveillance) or a brief course of treatment with a combination of drugs may be indicated for stage 1 non-seminomas.
Three to four cycles of chemotherapy, utilising a combination of various drugs, are administered for stage 2 and 3 testicular malignancies.
Following chemotherapy, additional surgery may be required to remove any damaged lymph nodes or deposits in the lungs or, in rare cases, the liver.
Some persons with stage 2 seminomas may be candidates for less intensive radiotherapy, which may be combined with a less aggressive form of chemotherapy.
Depending on the extent of the tumor’s spread, extra surgery may be required following chemotherapy to remove tumours from other regions of the body in non-seminoma germ cell tumours.
It can be tough to choose which treatment is best for you. Your oncology team will provide suggestions, but you will make the final decision.
You might find it helpful to develop a list of questions to ask your specialist before discussing your treatment options.
For example, you might wish to learn about the benefits and drawbacks of certain treatments.
If testicular cancer is discovered early enough, an orchidectomy may be the only therapeutic option.
An orchidectomy does not take place in the scrotum. The testicle, as well as all the tubes and blood arteries linked to the testicle that runs through the groyne into the abdomen, are removed through a cut in your groyne. The procedure is performed under a general anaesthetic.
You can have a prosthetic (artificial) testicle put into your scrotum to mask the look of your testicles.
Silicone, a soft form of plastic, is commonly used for prosthetic testicles. It won’t look exactly like your former testicle or the one you have now. It could be a little different in terms of size or texture.
Although you may need to stay in the hospital for a few days after an orchidectomy, you can usually be discharged quickly. If only one testicle is removed, there should be no long-term consequences.
You will be infertile if both testicles are removed (a bi-lateral orchidectomy).
However, removing both testicles at the same time is extremely uncommon, with only one out of every 50 instances necessitating the removal of the other testicle at a later date.
Before having a bilateral orchidectomy, you may be able to bank your sperm to allow you to father children if you so desire.
Banking of sperm
After one testicle is removed, the majority of people remain fertile. However, some testicular cancer therapies can result in infertility.
Because of alterations in the testicles that occur before the disease starts, some persons with testicular cancer may have poor sperm counts.
The capacity to ejaculate may be harmed in persons who need post-chemotherapy removal of tumours in the back of the abdomen, known as retroperitoneal lymph node dissection (RPLND), even if the surviving testicle can still generate sperm.
You might wish to think about sperm banking before you start your therapy.
A sample of your sperm is frozen so that it can be utilised to fertilise your partner during artificial insemination at a later date.
You may be asked to get HIV, hepatitis B, and hepatitis C testing before sperm banking.
You should always be given sperm banking if you’re undergoing complicated treatment for stage 2 or 3 testicular cancer. If you’re worried about your fertility, let them know.
Not every man is a good candidate for sperm banking. The sperm must be of reasonable quality for the technique to succeed.
There may also be instances where delaying therapy to allow for sperm banking is deemed too risky.
The majority of cancer treatment centres provide a free sperm bank. However, it is up to each region of the country to decide whether sperm storage is free or not.
Infertility may occur as a result of some treatments, like chemotherapy, but typical chemotherapies have a less than 50% probability of inducing infertility if the remaining testicle is normal.
Testosterone replacement therapy
If you have a healthy testicle left, it should produce enough testosterone for you to notice no change.
You may suffer symptoms caused by a shortage of testosterone if you have any difficulties with your remaining testicle.
These symptoms can be caused by a variety of factors, including:
- Tiredness
- Gaining weight
- Libido deficiency (sex drive)
- Beard growth is slowed
- Diminished ability to get and keep an erection (erectile dysfunction)
When both testicles are removed, you will no longer be able to produce testosterone and will experience the symptoms listed above.
Testosterone replacement therapy entails getting testosterone in the form of an injection, a skin patch, or a gel that you massage on your skin.
Injections are normally given every 2 to 3 months if you have them.
You’ll be able to keep an erection and your sex drive will improve after testosterone replacement therapy.
This sort of medication has few adverse effects, and if you do have any, they will usually be minor.
They may include the following:
- Oily skin, which can occasionally lead to acne breakouts
- Swelling and expansion of the breasts
- An enlarged prostate gland that exerts pressure on your bladder causes a shift in regular peeing habits, such as the urge to pee more frequently or having trouble peeing.
Lymph node and lung surgery
Testicular cancer can spread to your lymph nodes in more advanced situations. The immune system of your body includes lymph nodes, which help protect you from illness and infection.
Under general anaesthesia, lymph node surgery is performed. The lymph nodes in your abdomen are the ones that are most likely to require removal.
The nerves around the lymph nodes can be injured in some situations, which means that instead of ejaculating semen from your penis during sex or masturbation, the semen returns to your bladder. Retrograde ejaculation is the term for this type of ejaculation.
You will still have an orgasm during ejaculation if you have retrograde ejaculation, but you will not be able to father a kid.
The use of drugs that tighten the muscles around the neck of the bladder to block the flow of semen into the bladder is one method of treating retrograde ejaculation.
Men who desire to start a family can have sperm extracted from their urine and used in artificial insemination or in vitro fertilisation (IVF).
Some persons with testicular cancer have cancer deposits in their lungs, which may need to be removed following treatment if they haven’t vanished or shrunk in size enough.
This sort of surgery is also performed under general anaesthesia and does not usually have a long-term impact on breathing.
Nerve-sparing retroperitoneal lymph node dissection
Because it has a lower chance of producing retrograde ejaculation and infertility, a newer type of lymph node surgery called nerve-sparing retroperitoneal lymph node dissection (RPLND) is becoming more popular.
The operation site is restricted to a substantially smaller area with nerve-sparing RPLND. This means that nerve injury is less likely to develop.
The procedure is more technically hard, which is a drawback.
RPLND that spares nerves is currently only offered at speciality centres with surgeons who have completed the necessary training.
Laparoscopic retroperitoneal lymph node dissection
The lymph nodes can be removed via laparoscopic retroperitoneal lymph node dissection (LRPLND), a sort of keyhole surgery.
The surgeon will make several little cuts in your tummy during LRPLND.
A device known as an endoscope is put into one of the cuts. An endoscope is a thin, long, flexible tube with a light and camera on one end that transmits images of the inside of your body to a television monitor.
Small surgical instruments are passed down the endoscope and can be used to remove the lymph nodes that are causing the problem.
The benefit of LRPLND is that it has a shorter recovery time and less postoperative pain.
In addition, unlike nerve-sparing RPLND, LRPLND has a lower risk of nerve injury leading to retrograde ejaculation.
However, because LRPLND is a novel treatment, there is limited information about its long-term safety and effectiveness.
If you’re thinking of getting LRPLND, keep in mind that there are still some questions about the procedure’s safety and effectiveness.
Radiotherapy
To help eradicate cancer cells, radiotherapy uses high-energy beams of radiation.
After surgery, seminomas may require radiotherapy to help prevent cancer from returning.
It may also be required in advanced situations where a patient is unable to withstand the sophisticated chemotherapies often used to treat testicular cancer in stages 2 and 3.
After a course of chemotherapy, you may need radiotherapy if your testicular cancer has progressed to your lymph nodes.
The following are some of the possible side effects of radiotherapy:
- Similar to sunburn, reddening and discomfort of the skin
- Feeling unwell
- Diarrhoea
- Fatigue
These adverse effects are usually just temporary, and they will go away once your therapy is finished.
Chemotherapy
Chemotherapy is a treatment that employs strong drugs to destroy or stop tumour cells from proliferating in your body.
If you have advanced testicular cancer or it has spread throughout your body, you may need chemotherapy. It’s also used to keep the cancer from coming back.
Seminomas and non-seminoma tumours are routinely treated with chemotherapy.
Chemotherapy for testicular cancer is frequently administered through a vein.
In other situations, a central line is utilised, which stays in a vein throughout your therapy and eliminates the need for blood tests or needles to be inserted into new veins.
Chemotherapy drugs can sometimes harm your body’s natural, healthy cells. As a result, it might have a wide range of adverse effects.
Among the most common are:
- Being unwell
- Feeling unwell
- Hair loss
- Ulceration in the mouth and sore mouth
- A decrease in appetite
- Fatigue
- Lung damage and dyspnea
- Infertility
- A ringing sensation in your ears (tinnitus)
- Skin that quickly bleeds or bruises
- A low platelet count
- Infection susceptibility has risen
- Tingling and numbness in your hands and feet (pins and needles)
- Renal failure
These adverse effects are usually relatively transitory and should go away once your therapy is over.
Side effects, like infections that arise when you have a low blood count, can be fatal, so you should always contact your cancer care team if you’re concerned in between chemotherapy treatments.
Bleomycin
Bleomycin, one of the most regularly used drugs, has been linked to long-term lung damage.
If damage to your lungs would have a specific impact on your profession or lifestyle, you should talk to your doctor about it.
However, the advice may still be that you should have it in order to have the best chance of getting better.
Having children
You should not have children while undergoing chemotherapy or for a year after it has ended.
Chemotherapy medicines might harm your sperm temporarily, raising your chances of fathering a child with major birth abnormalities.
During this period, you’ll need to utilise a dependable means of contraception, such as a condom.
Condoms should also be worn for the first 48 hours after a chemotherapy treatment.
This is to keep your spouse safe from the chemotherapy medicine in your sperm.
Learn more about chemotherapy’s side effects.
Follow-up
There’s a chance your cancer will come back, even if it’s been entirely cured.
The likelihood of your cancer returning will be determined by the stage at which you were diagnosed and the therapy you had since then.
The majority of non-seminoma testicular cancer recurrences happen within two years of surgery or chemotherapy.
Recurrences in seminomas might last up to three years. Recurrences beyond three years are uncommon, occurring in less than 5% of patients.
You’ll need regular testing to see if cancer has returned due to the danger of recurrence.
These are some of them:
- A physical examination
- Blood tests to check for tumour markers
- A chest X-ray
- A CT scan
Depending on the degree of the malignancy and the treatment options, follow-up and testing are frequently necessary.
The first year or two are usually the most frequent, although follow-up consultations might last up to five years.
In some situations, follow-up appointments may be required for a period of 10 years or longer.
If cancer returns after treatment for stage 1 testicular cancer and are detected early enough, it can usually be cured with chemotherapy and possibly radiotherapy.
Recurrent testicular cancer has a cure rate of above 95% in some cases.
Recurrences that occur after previous combination chemotherapy can also be treated, but the chances of this vary from person to person, so talk to your doctors about it.
Complications of testicular cancer
Testicular cancer, despite being extremely curable, can nevertheless spread to other regions of the body.
Your fertility may be compromised if one or both testicles are removed.
Before you start treatment, talk to your doctor about your fertility preservation options.
SUMMARY
Cancer of the testicles is known as testicular cancer. It can spread outside of the testicle and into other regions of the body, known as metastasis. Testicular cancer is a rare disease, accounting for about 1% of all cancers in males. Each year, approximately 2,300 males in the United Kingdom are diagnosed with testicular cancer.
Young and middle-aged men are more likely to get testicular cancer, which is often successfully treated with a combination of surgery, chemotherapy, and radiation therapy.
Testicular cancer has a very high 5-year survival rate, with a 98 percent overall survival rate.


